Dropping an ice crystal into a bottle of near-frozen water produces a dramatic effect: very quickly, the liquid crystallizes into a block of ice.
At the molecular level, an ice crystal has a distinct shape—a lattice structure. As incoming water molecules reshape to join the lattice, the crystal grows.
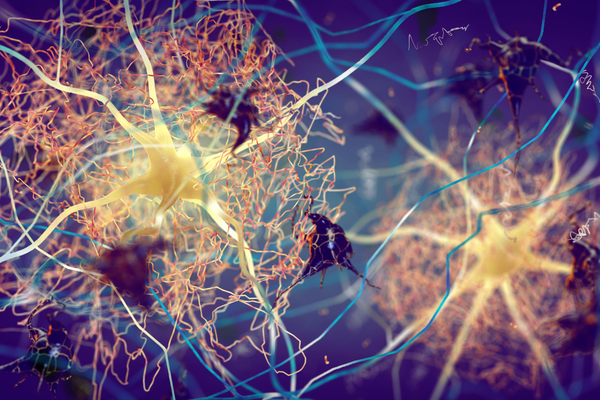
Some researchers think an analogous process underlies Alzheimer’s disease, Parkinson’s disease and other neurodegenerative illnesses. According to this theory, these diseases begin when a particular protein misfolds, or fails to assume the proper shape for its intended role. That misshapen molecule ensnares normal versions of the protein, causing them to similarly misfold, and over time, these rogue proteins clump into toxic clusters that spread through the brain.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
In mad cow disease—a brain disorder in cattle that can spread to people who eat meat from ill animals —the toxic proteins, called prions, ravage the mind quickly, leading to dementia and death within months. Prion diseases are rare. About 350 cases of the most common type, Creutzfeldt-Jakob disease, are reported each year in the U.S.
By comparison, each year, nearly 500,000 people in the U.S. are diagnosed with Alzheimer’s, which develops more gradually. Plaques made up of abnormal beta-amyloid proteins can accumulate in the brain for years or even decades before a person notices signs of mental decline.
While the time lines for toxicity differ, “the mechanism of misfolding is the same,” says Mathias Jucker, a neuroscientist at the Hertie Institute for Clinical Brain Research at the University of Tübingen in Germany. Just as all of the water in a bottle freezes after a “‘misfolded’ water molecule” slips into the vessel, if “you have one misfolded protein, all the other ones will take the same shape.”
The idea that many diseases could arise from a common prionlike process raises an intriguing and troubling question: Under certain circumstances, could neurodegenerative disorders be transmitted from person to person?
Scattered studies in the past decade suggest that this could be possible, but such events seem exceedingly rare, and scientists are still working out how the pathogenic seeds originate and spread.
A small 2015 study gave one of the first strong hints that misfolded beta-amyloid could pass from one person to another. Analyzing autopsy tissue from eight people who died of Creutzfeldt-Jakob—in whom the disease had surfaced decades after they had received childhood injections of human growth hormone extracted from the pituitary glands of cadavers—researchers noticed that six of them had, in addition to the disease, an abundance of amyloid plaques. Such a heavy buildup of brain amyloid in people who had died so young—between the ages of 36 and 51—was surprising.
The team then dug up old stocks of growth-hormone preparations and found them to be contaminated with beta-amyloid and another protein called tau, which is also a pathological hallmark of Alzheimer’s disease. When the researchers injected these growth-hormone preparations into the brains of young mice that were engineered to model Alzheimer’s disease, this spurred amyloid buildup, whereas plaques failed to form in control mice that had received pure growth hormone that didn’t come from the cadavers of people who died of Creutzfeldt-Jakob.
Those findings, published in 2018, suggested the preparations contained beta-amyloid “seeds” that could spread between people in certain conditions. In a separate set of mouse experiments, Jucker and his colleagues showed that such “seeds” retain potency even after sitting dormant in the brain for months.
Other reports of rare instances where beta-amyloid seeds seemingly passed between people have cropped up sporadically through the years. Some research focuses on cerebral amyloid angiopathy (CAA), a condition marked by amyloid buildup in cerebral blood vessels. Scientists think CAA could increase the risk of microbleeds that develop in the brains of some people with Alzheimer’s who are treated with antibodies to remove amyloid.
These reports document early-onset CAA in a handful of adults who previously received grafts from cadavers to patch holes in membranes that surround the brain and spinal cord. Another study combed pathology archives and medical literature and found cases of CAA that had occurred at unusually young ages in eight adults who had undergone brain surgery during their childhood or teen years. These analyses raise the possibility that beta-amyloid seeds unwittingly entered people’s brain via contaminated surgical tools.
A group of scientists did a more concerted search—focusing on blood transfusions and more common neurosurgeries—and turned up 11 CAA cases with suspected beta-amyloid transmission through neurosurgeries but none from blood transfusion during those procedures.
In September a team at Karolinska University Hospital in Sweden published circumstantial evidence that seemed to suggest that blood transfusions could transmit beta-amyloid. The scientists scoured the medical records of more than a million people and found that those who received blood from someone who later developed multiple microhemorrhages were about three times more likely to suffer a brain bleed in the next several years.
Interest in disease transmission through pathological seeding is also sustained by occasional tragic news from the research community. Last month the University of Barcelona announced that it had opened an investigation to track the origins of unauthorized lab samples that may have contributed to the death of a biochemist studying Creutzfeldt-Jakob disease.
Scientists are still struggling to understand fundamental details about prionlike disease transmission—for example, what sparks the initial misfolding event. “It’s elusive,” says Henrik Zetterberg, a neurochemist at the University of Gothenburg in Sweden.
Without technology to visualize misfolded proteins in the brains of living people, “we will never know,” Jucker says.
Jucker describes two possibilities: One is that formation of the initial aggregate is an extremely rare event—so rare that it’s unlikely to happen until a person is well on in years. The second possibility is that protein aggregates form routinely even in youth but don’t cause problems because the abnormal clusters get cleared out through normal metabolic processes. This clearance system slows down with age, however, making older people more vulnerable to the buildup of misfolded proteins, which can then spread and propagate disease.
These mechanisms are “fundamentally different,” Jucker says. “But in the end, it’s the same. Propagation starts when you are old.” In both cases, the instigating agent is initially undetectable by positron-emission tomography (PET) imaging.
With more recent advances in a sophisticated imaging technique called cryo-electron microscopy (cryo-EM), it is possible to distinguish the same protein when it adopts distinct conformations. Using cryo-EM to examine autopsy tissue from people with various diseases that resulted in a buildup of the tau protein, researchers have been able to detect distinct shapes of misfolded tau that are associated with different diseases. Similarly, scientists have found differences in the folding patterns for another protein called alpha-synuclein, which aggregates in Parkinson’s and other diseases.
These ideas have therapeutic implications. Even when pathologies are not yet detectable, as is the case with young Alzheimer’s model mice that have not yet shown signs of buildup, Jucker and his co-workers have shown that treatment with amyloid antibodies substantially delays the formation of amyloid plaques in the brains of these mice. These findings give an indirect suggestion that beta-amyloid “seeds” were cleared. The results also jibe with Alzheimer’s disease trials of newly approved amyloid antibodies, which show that removing brain amyloid can slow cognitive decline and suggest that intervening even earlier could potentially prevent amyloid buildup in the first place. Prevention “is the obvious next frontier,” says Lary Walker, a neuroscientist at Emory University, who co-authored a recent review on this topic with Jucker.
The basic molecular mechanism underlying the misfolding of these proteins applies to numerous disorders. But the different diseases have distinctive primary proteins—the ones that initiate the pathological process. Each of them differs in their toxicity and ability to spread. Using high-resolution microscopy to analyze cultured neuronal cells, some researchers have observed alpha-synuclein aggregates spreading from cell to cell within dynamic structures called tunneling nanotubes.
Ultimately, much about prionlike disease processes remains a mystery. Even with numerous reports suggesting “infectivity,” or transmission of disease pathology from one organism to another, “we don’t know what the infectious unit is,” Jucker says. For example, in the ice crystallization analogy, researchers still puzzle over the exact nature of the pathogenic “seed.” Is it “the ice [that] has been generated,” Jucker asks, “or is it the invisible seeds, which are still in this beaker, and the ice is just the end product?”